You might have undergone an operation.
You might have poor general health.
Or, simply, you just don’t want conservative treatment or its allied complications.
Reasons could be any. And, all of them are valid to choose a non-surgical option if you’ve been diagnosed with pelvic organ prolapse (POP).
Surgery is obviously the last resort, and hopefully you may not need to experience that stage. If you start the treatment in the early stages, you’ll not just end up strengthening your pelvic muscles but also get rid of emotional heaviness.
As a pelvic floor physiotherapist, I often come across many questions from patients in Ontario. Some sound confused, while some are hesitant. So to make you confident, this guide has been made.
Pelvic Organ Prolapse (POP): What Does It Mean?
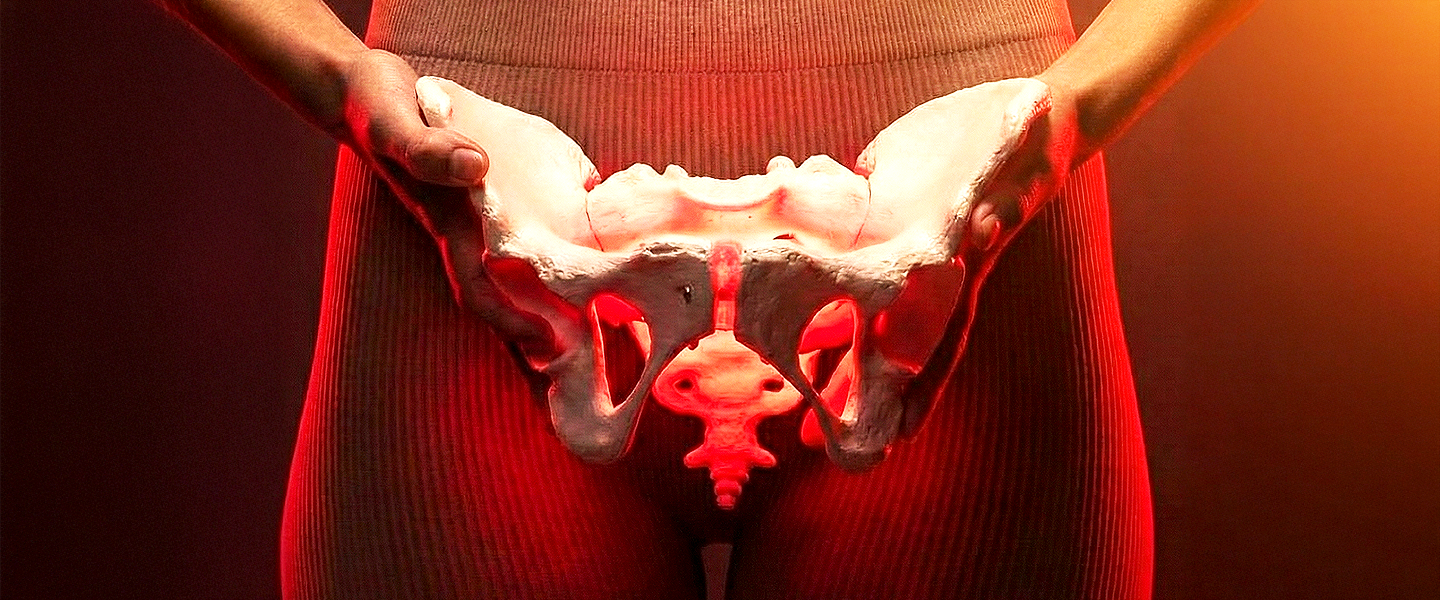
Your pelvic floor contains muscles from the pubic bone to the tailbone. It supports your pelvic organs, including bladder, bowel, anus, urethra, and rectum. When they’re weakened, overly tight, or strained, we call the situation Pelvic Organ Prolapse.
Especially in women, in a mild case, pelvic floor muscles slightly drop from their original position. But in a severe case of pelvic floor pain they feel the bulge as if something is falling out from their vagina. Though POP is more commonly found in women, men are not also out of it. Rare, but they can also experience the rectal or bladder prolapse.
So, I jotted down the type of prolapse that you may have seen. They include:
- Cystocele: Cystocele or bladder prolapse involves the descent or sagging of the bladder into the vaginal canal.
- Urethrocele: This condition results from the bulging of the urethra (where urine exits the body) into the front vaginal wall.
- Vaginal vault prolapse: It usually occurs after a hysterectomy. It is described as the prolapse of the top part of the vagina into the vaginal canal.
- Enterocele: In this type of prolapse, the weakened muscle of the small intestine either bulges onto the back wall or the top of the vagina.
- Rectocele: This condition involves the wall at the front of the rectum bulging into the back of the vagina.
- Uterine prolapse: As the womb falls into the vaginal canal, this causes profound effects on disrupting your bowel and urinary function. It can also protrude out of the body in a severe case.
How is Pelvic Organ Prolapse Diagnosed?
To confirm whether you have an acute or chronic prolapse condition, we need to diagnose it. We follow several steps in our pelvic organ prolapse pessary fitting clinic in Ontario, including
- Routine Pelvic Exam: Your doctor will examine you while you are lying down and often while you are standing. He might ask you to bear down or cough to see if a particular organ or more has slipped out of the place.
- POP-Q (Pelvic Organ Prolapse Quantification): In this examination, stage 0 indicates no prolapse, while Stage IV means complete prolapse. This helps identify the degree of descent of pelvic organs from the hymen.
- Imaging test: In a complex case, you may be asked to ultrasound or a dynamic pelvic MRI to check pelvic organs movement in real-time.
- Urodynamics: While measuring pressure and volume in urinary incontinence or emptying of the bladder, this test helps find the root cause.
- Cystoscopy: This test helps find out other internal obstructions or bladder issues that are mainly caused by prolapse. However, it isn’t directly involved to diagnose prolapse.
Is There Any Non-Surgical Treatment for Pelvic Prolapse Support Available in Ontario?
Pelvic Floor Muscle Training (PFMT)
Let’s start with a very common method, pelvic floor exercises EKA Kegel exercises. Like many others, you may have already tried to manage prolapse. However, results may be limited if you don’t practice them consistently every day. Many women also mistake them as a complete solution, even in cases of severe prolapse. In reality, they are most effective for mild prolapse symptoms such as slight abdominal pressure and bladder leakage.
To get the most out of this pelvic floor exercise (EKA Kegel exercises), try an electronic pelvic toner. Also, a biofeedback machine can be handy to track your progress. Moreover, if you could practice exercises under the guidance of an experienced pelvic floor physiotherapist, what could be better than this? Altogether, this will help you to manage your pelvic prolapse symptoms and strengthen muscles over time.
Fitting Vaginal Pessary
This has become the fastest option among women who have mid to moderate pelvic organ prolapse. Initially, your healthcare professional inserted a small, soft silicone device into your vagina.
While a ring or cube pessary can be your first line option, its structure may differ into advanced cases.
However, here, an important thing to remember is that a vaginal pessary can manage your prolapse symptoms and help improve your daily life activities. But it never cures any structural damage. Also, you should avoid a vaginal pessary fitting if you’re pregnant, and it can be used following childbirth.
Be confident to insert, remove, or clean this pessary on your own. To take extra care, you can follow up with your healthcare professional around every six months. Communicate openly with them when you feel sharp pain, odor, or vaginal discharge after fitting a pessary. It’ll help your healthcare professional to modify ongoing support for you.

Lifestyle Changes
Last but not the least, modification in your lifestyle can make a great impact while choosing non-surgical pelvic prolapse support. So what can you do?
- Make a habit of consuming vitamin D3 and K2 combined supplements daily.
- Include fibre-rich bowls and ample amounts of water in your diet.
- Avoid straining and holding your bladder and bowel movement.
- Maintain a perfect posture and change motion during workouts, and avoid prolonged sitting.
- Do not engage in heavy lifting that your body can’t support.
A Note from the Physiotherapist of Get Back Physiotherapy Clinic in Ontario
The surgical or non-surgical prolapse treatment isn’t for all. It completely depends on what kind of prolapse you’ve faced, or how strong your pelvic muscles are. Based upon the diagnosis, your treatment is decided.
However, when it comes to the expertise, skilled, and supportive care, you can connect and book your appointment with Get Back Physiotherapy. At our women’s pelvic floor physiotherapy clinic at Mississauga, we provide postpartum, prenatal pelvic, and incontinence pelvic floor physiotherapy alongside a non-surgical pessary fitting treatment. You can expect just not the treatment but emotional support throughout.
FAQs
Q1: What are the non-surgical treatments for prolapse?
Ans: Pelvic floor muscle training (PMFT), Kegel exercises, vaginal pessary fitting, and pelvic floor physiotherapy are some really good non-surgical treatment options to fix your prolapse. You can get it with us at Get Back Physiotherapy, the women’s pelvic floor physiotherapy in Mississauga.
Q2: How to fix a prolapsed bladder without surgery?
Ans: By fitting a vaginal pessary, and in some cases with oestrogen replacement therapy, your prolapsed bladder can be fixed without surgery. However, a pessary is definitely non-risky, while hormone replacement therapy (HRT) is associated with risks.
Q3: Can a pessary fitting be the permanent cure for my POP?
Ans: Not really. While it can prevent worsening your prolapse, it cannot fix structural damage. A pessary can be used to treat your chronic pain, burning sensation, or the feeling of something falling out of your vagina.
Q4: When is surgery necessary for my POP treatment?
Ans: Surgery can be your last option when non-surgical treatment fails to improve conditions as expected. In this case, your healthcare professional in Ontario can guide you better after assessing your medical condition.
Q5: What to expect in my first appointment with a pelvic floor physiotherapist in Ontario?
Ans: When you visit us for your on-surgical pelvic prolapse support in Ontario, we start with assessing your medical history, general health condition, and routine pelvic exam. Further, we move forward to the treatment such as exercises, physical therapy, or pessary fitting, that best works to strengthen your pelvic muscles. Throughout the process, we do it with utmost respect, care, and emotional support.