Understanding Real Outcomes Beyond Simple Promises
Most content about pelvic floor physiotherapy makes it sound straightforward. You’ll find lists of exercises, general reassurance, and the repeated promise that strengthening fixes everything. But that’s not how real outcomes work in clinical practice.
This comprehensive guide explains what pelvic floor physiotherapy actually accomplishes, identifies where it works well and where it falls short, and reveals why many women don’t improve despite following every recommendation perfectly. This isn’t about theory—it’s about understanding the decision logic that determines your results.
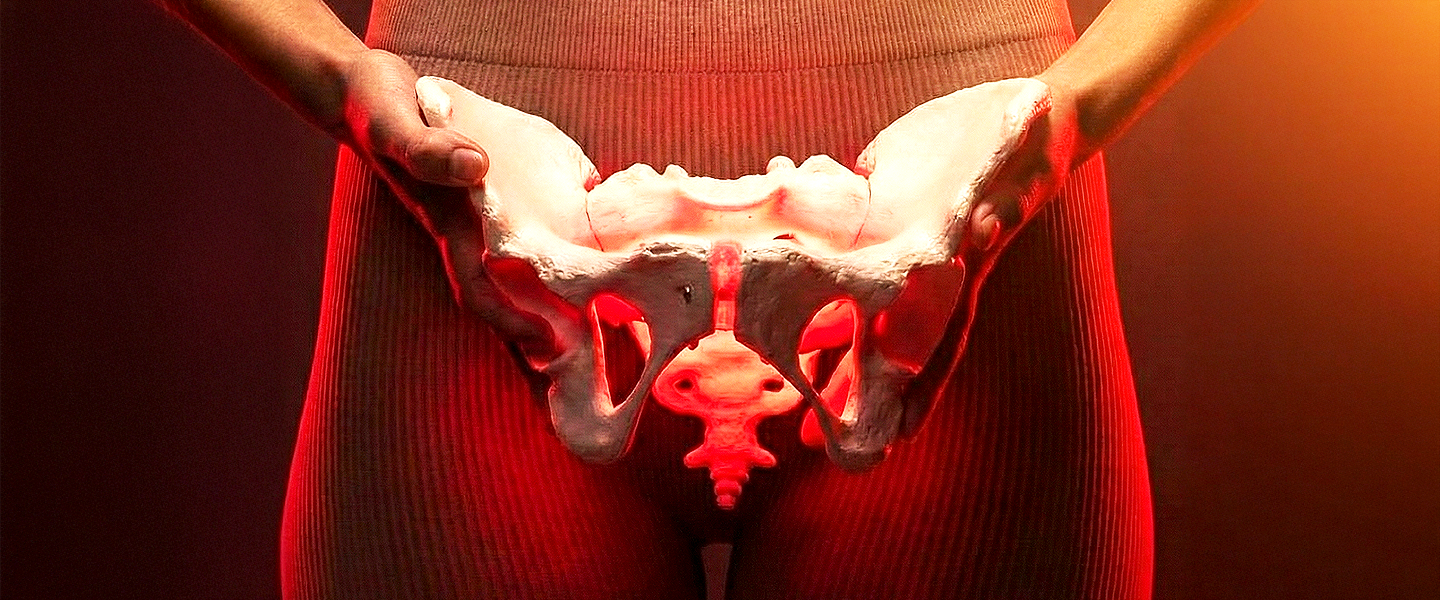
Why Pelvic Floor Issues Are Never Isolated Problems
The Fundamental Misunderstanding
Most competitor blogs treat the pelvic floor like a standalone muscle group that simply needs strengthening. This oversimplified view misses the core reality of how your body actually functions.
In clinical reality, the pelvic floor behaves more like a sophisticated pressure management system. It doesn’t work in isolation—it coordinates constantly with your breathing patterns, core muscles, hip mechanics, and spinal alignment to manage forces throughout your entire body.
What Disrupts This Complex System
Multiple factors can throw off this delicate coordination. Pregnancy changes your center of gravity and floods your system with hormones that alter tissue elasticity. Delivery—whether vaginal or cesarean—creates significant disruption through stretching, tearing, or surgical cutting. Hormonal shifts throughout life stages affect how tissues respond to load. Surgery creates scar tissue that restricts normal movement patterns. Pain causes you to move differently, creating compensations. Even chronic stress fundamentally changes your breathing mechanics in ways that impact pelvic floor function.
When this integrated system breaks down, symptoms often appear far from the actual source of the problem. This is the key insight most surface-level advice completely misses.
Understanding Confusing Symptom Patterns
This system-wide disruption explains why women experience seemingly contradictory presentations that don’t make sense if you’re thinking about simple muscle weakness.
Common Confusing Patterns:
What You Experience | What It Seems Like | What’s Actually Happening |
Leaking during activity | Muscle weakness | Timing and coordination failure |
Pelvic pain | Tissue injury | Overactivity or nervous system threat response |
Prolapse symptoms | Sudden trauma event | Gradual pressure system breakdown |
Muscle tightness | Need to stretch more | Muscles protecting or compensating |
These patterns reveal that the problem isn’t just about strength. It’s about how the entire system coordinates under pressure.
When Pelvic Floor Physiotherapy Actually Makes a Difference
The Success Formula
Pelvic floor physiotherapy for women is most effective when the problem is functional rather than purely structural. Functional problems involve how the system coordinates and responds. Structural problems involve tissue damage that may be beyond the scope of conservative treatment.
Understanding this distinction is critical for setting realistic expectations about what physiotherapy can and cannot accomplish.
Conditions That Respond Well to Treatment
Postpartum Recovery Needs
Whether you had a vaginal delivery or C-section, your body needs to relearn coordination patterns that pregnancy and delivery disrupted. The changes aren’t just about tissue damage—they’re about how your nervous system controls muscle timing and pressure management.
Urinary Incontinence Driven by Coordination Loss
When your pelvic floor doesn’t contract at the right moment relative to pressure spikes, physiotherapy can retrain this anticipatory timing. This is fundamentally different from simple weakness, though the symptom looks the same.
Painful Intercourse Linked to Muscle Guarding
If your muscles tense protectively in response to perceived threat, therapy can help them learn to relax appropriately. This involves nervous system retraining, not just local muscle work.
Early-Stage Pelvic Organ Prolapse
When tissue support can still adapt and symptoms are in mild to moderate stages, physiotherapy improves how your body manages pressure to reduce symptoms and potentially slow progression.
The Critical Factors That Determine Success
Success doesn’t come from exercise selection alone. Three factors determine whether treatment creates meaningful change.
FACTOR ONE: Timing
When You Start Treatment | Impact on Outcomes | Why |
Early intervention (weeks 2-8 postpartum) | Highest success rate | Compensation patterns haven’t become ingrained habits |
Delayed intervention (3-6 months) | Moderate success rate | Some compensatory strategies exist but are still modifiable |
Late intervention (6+ months) | More challenging | Deep compensatory habits require significant retraining |
FACTOR TWO: Load Management
Improvement depends on gradually building your capacity to handle real-world demands. This isn’t about avoiding activities indefinitely or jumping back to full activity immediately. It’s about progressive exposure that builds tissue tolerance and nervous system confidence.
FACTOR THREE: Nervous System Response
Your brain and muscles must relearn how to communicate effectively under pressure. Conscious control during exercises is just the starting point—the real goal is automatic, anticipatory control during daily activities.
Postpartum Recovery—The Complete Picture
Beyond the “Just Get Strong Again” Myth
Postpartum pelvic floor therapy is typically reduced to a simple narrative: delivery weakened your muscles, so you need to strengthen them again. This narrative is fundamentally misleading.
After delivery, your pelvic floor doesn’t just lose strength. More importantly, it loses timing. The muscles can’t respond quickly enough when pressure suddenly increases from coughing, lifting, or even standing up from a seated position.
Consider the time gap: a cough creates a pressure spike in approximately 0.2 seconds. A conscious muscle contraction takes 0.5 to 1.0 seconds to fully develop. Your muscles are literally too slow to respond, even if they’re technically strong enough. This timing deficit explains why leakage and heaviness persist even in women whose muscles test as “strong” during clinical examination.
Why Jumping Straight to Exercises Can Backfire
Many women start strengthening exercises immediately after delivery, often at the recommendation of well-meaning healthcare providers or online resources. This approach frequently makes symptoms worse rather than better.
You’re attempting to strengthen a system that hasn’t yet relearned how to manage pressure appropriately. It’s like trying to run before you’ve relearned to walk after a neurological injury—the strength might be adequate, but the coordination isn’t ready.
The Correct Progression Sequence
PHASE ONE: Foundation Building (Weeks 1-6)
This early phase focuses on reestablishing basic coordination rather than building strength. You need to relearn how breathing coordinates with pelvic floor activation, develop awareness of abdominal pressure patterns during daily activities, and begin gentle whole-body movement that doesn’t challenge the system beyond its current capacity.
The exercises in this phase should feel easy. If they’re challenging, you’re likely pushing too hard too soon.
PHASE TWO: System Integration (Weeks 6-12)
Once basic coordination is reestablished, you can begin integrating the pelvic floor with hip and trunk participation. This phase introduces coordination under light load, retrains daily activity patterns like lifting, bending, and transitioning between positions, and gradually increases complexity without exceeding tissue capacity.
The goal isn’t maximum strength—it’s reliable function under typical daily demands.
PHASE THREE: Progressive Loading (Week 12 and Beyond)
Only after the first two phases are solid should you progress to graduated return to exercise, task-specific training for activities you want to resume, and deliberately building confidence and tissue capacity through progressive overload.
This phase looks most like traditional strengthening, but it only works because the foundation was properly established first.
The Connection to Whole-Body Function
The pelvis rarely fails in isolation. Postpartum recovery parallels what we see in lower back pain rehabilitation, hip dysfunction treatment, and core stability restoration. Problems in any of these areas create compensations that affect pelvic floor function, and pelvic floor dysfunction creates compensations that affect these other areas.
This is why isolated pelvic floor exercises often fail—they ignore the interconnected system that must function as a coordinated whole.
C-Section Recovery—Debunking the “No Trauma” Myth
The Dangerous Assumption
Many women and healthcare providers assume that having a C-section means you won’t have pelvic floor issues since you didn’t have vaginal trauma. This assumption is dangerously wrong and leads to missed opportunities for early intervention.
Understanding the Impact Chain
Surgical Incision Through Abdominal Wall
↓
Disruption of Seven Tissue Layers
↓
Scar Tissue Formation Restricts Movement
↓
Altered Pressure Transfer Patterns
↓
Compensatory Movement Strategies Develop
↓
Pelvic Floor Indirectly Overloaded
↓
Delayed Symptoms Appear (3-6+ Months Later)
The abdominal wall disruption from surgery fundamentally alters how pressure transfers through your core during every activity—breathing, moving, lifting, even laughing. Scar tissue restricts normal muscle sequencing and changes the timing of muscle activation patterns. Your body develops protective movement strategies to avoid pain or pressure at the incision site, and these strategies often overload the pelvic floor indirectly.
Why Symptoms Appear Months Later
Women frequently develop pain, heaviness, or urinary symptoms three to six months after C-section, not immediately following surgery. By this point, compensatory movement habits are deeply ingrained and significantly harder to modify than if they’d been addressed early.
This delayed presentation creates a false sense of security. Women think they’ve “escaped” pelvic floor problems, then symptoms develop unexpectedly months later when protective habits can no longer compensate for the underlying dysfunction.
The Critical Window for Intervention
This mirrors what we consistently see in pre and post-operative rehabilitation across all surgical procedures: delayed dysfunction is exponentially harder to unwind than early correction. The window for easiest intervention is weeks two through eight, before compensation patterns become automatic habits.
Pelvic Organ Prolapse—Realistic Expectations
What Physiotherapy Can Accomplish
Pelvic organ prolapse physiotherapy works best in early to moderate stages. Understanding what it can and cannot do is essential for making informed treatment decisions.
Realistic Capabilities:
- Improve the timing of muscle support so the pelvic floor engages more effectively during pressure increases
- Reduce symptom severity so daily activities become more comfortable and manageable
- Slow the rate of progression, though not necessarily prevent it entirely
- Restore confidence in movement and activity so fear doesn’t become the primary limiting factor
- Improve overall quality of life through better symptom management strategies
What Physiotherapy Cannot Do
Many blogs avoid this honest conversation, but you deserve to understand the realistic scope of conservative treatment.
Limitations of Conservative Care:
- Cannot reverse advanced tissue descent that has already occurred
- Cannot compensate for daily loads that consistently exceed your body’s capacity to manage
- Cannot replace surgical intervention when it’s medically indicated based on symptom severity or tissue changes
- Cannot “cure” structural changes that are beyond the scope of functional adaptation
Understanding Why Treatment Succeeds or Fails
Success Factors in Prolapse Management:
Treatment succeeds when it addresses whole-body mechanics rather than isolating the pelvic floor, builds load tolerance progressively through graded exposure, includes functional activities that matter for daily life, manages expectations realistically from the start, and integrates pressure management into everything you do.
Failure Factors in Prolapse Management:
Treatment fails when exercise programs ignore the actual loads you face in daily life, when healthcare providers tell you to “avoid everything” indefinitely, when fear becomes the primary driver of your movement choices, when treatment isolates the pelvic floor without addressing core and hip function, and when expectations are unrealistic about what conservative treatment can accomplish.
The Load Tolerance Principle
FAILURE CYCLE:
Symptoms → Avoid All Activity → Gradually Lose Capacity →
Eventually Resume Activity → Symptoms Return Worse
VERSUS
SUCCESS CYCLE:
Symptoms → Understand Triggers → Gradual Controlled Exposure →
Build Tissue Tolerance → Progressively Increase Activity →
Manage Symptoms Within Acceptable Range
Long-term outcomes depend on building load tolerance through progressive exposure, not on avoiding load indefinitely. Avoidance provides temporary symptom relief but guarantees long-term capacity loss.
Painful Intercourse—Why Strengthening Often Backfires
Flipping the Traditional Framework
Painful intercourse linked to the pelvic floor is rarely about weakness, despite what traditional advice suggests. More commonly, it stems from muscles that are overactive and can’t relax appropriately, a nervous system that perceives threat and maintains protective tension, or poor relaxation capacity under the specific demands of sexual activity.
Understanding the Strengthening Trap
Starting Point: Overactive Muscles
↓
Add Strengthening Exercises
↓
Muscle Tone Increases Further
↓
Pain Intensifies
↓
Do More Exercises (assuming they’re “not working yet”)
↓
Significantly Worse Pain
When you strengthen muscles that are already overactive, you increase muscle tone. Higher tone in this context increases pain rather than resolving it. This creates a frustrating cycle where more effort produces worse outcomes.
This is where many resources default to recommending “reverse Kegels” without adequately explaining when they help, when they don’t, and what else needs to be addressed beyond just the pelvic floor muscles themselves.
The Root Causes in Order of Frequency
Primary Issue: Overactive Muscles
The pelvic floor maintains excessive resting tone and cannot relax appropriately during activities that require length and compliance. This isn’t weakness—it’s the opposite problem.
Secondary Issue: Threat Response
The nervous system perceives sexual activity as threatening based on previous pain experiences, creating automatic protective muscle tension that’s not under conscious control.
Tertiary Issue: Poor Relaxation Capacity
Even when consciously trying to relax, the muscles cannot adequately lengthen and soften under the specific pressure and movement demands of intercourse.
What Actually Works for Pain-Related Dysfunction
Treatment Hierarchy for Painful Intercourse:
Step 1: Nervous System Calming
↓
Step 2: Learning to Relax Muscles Consciously
↓
Step 3: Gradual Exposure Therapy to Reduce Threat Perception
↓
Step 4: Breathing and Trunk Coordination Training
↓
Step 5: Manual Therapy When Indicated
↓
Step 6: Gentle Strengthening (Final Step, Only If Needed)
Effective care requires graded exposure protocols that gradually reduce nervous system threat perception, nervous system down-regulation techniques that calm protective responses, breathing and trunk coordination that distributes load appropriately, and manual therapy input when soft tissue restrictions limit progress.
This approach overlaps significantly with chronic pain treatment principles. Pain in this context isn’t just about tissue—it’s about how your nervous system interprets and responds to signals.
Urinary Incontinence—The Coordination Problem
Understanding Why Daily Exercises Aren’t Enough
Successful urinary incontinence treatment depends on your pelvic floor contracting before pressure spikes occur, not after. This distinction is critical and explains why traditional exercise approaches often fail.
The Speed Gap Problem
TIME TO GENERATE PRESSURE SPIKE:
Cough, Laugh, or Jump = 0.2 seconds
TIME TO CONSCIOUSLY CONTRACT:
Deliberate Muscle Activation = 0.5 to 1.0 seconds
THE PROBLEM: YOUR CONSCIOUS CONTROL IS TOO SLOW
Coughing, laughing, and running happen faster than you can consciously contract your muscles. This is the fundamental reason why many women continue leaking despite doing pelvic floor exercises faithfully every single day. They’re training conscious control when what they need is automatic, anticipatory control.
What Creates Real Improvement
Anticipatory Control Development
Training your nervous system to engage muscles automatically before sudden pressure increases, without requiring conscious thought or deliberate activation. This is fundamentally different from the voluntary contractions you practice during exercises.
Whole-Body Coordination
Ensuring your trunk, hips, and breathing mechanics all participate appropriately rather than putting all the demand on your pelvic floor alone. When the system shares the load, no single component gets overwhelmed.
Task-Specific Retraining
Practicing the actual activities where you leak—coughing, jumping, running—not just isolated exercises in non-challenging positions. The nervous system learns through specific practice of the exact tasks that matter.
The Sports Performance Parallel
This follows the same logic as sports injury prevention. Systems fail when timing fails, not necessarily when strength is inadequate. You can have all the strength in the world, but if it’s not available at precisely the right moment, it doesn’t help.
Three Critical Truths Other Resources Won’t Tell You
Truth One: Strength Is Rarely Your Primary Limiting Factor
Many women already have adequate pelvic floor strength when formally tested. The problem isn’t muscle weakness—it’s the inability to access and use that strength effectively under real-world conditions and timing demands.
Clinical testing in a controlled environment doesn’t replicate the demands of sudden pressure spikes during daily life. You might test as “strong” but still experience symptoms because strength alone isn’t sufficient.
Truth Two: Isolating the Pelvic Floor Creates New Problems
When treatment focuses exclusively on the pelvic floor without addressing your hips, spine, and breathing mechanics, you develop compensation patterns that create new problems in other areas.
We consistently see these compensations show up as knee pain, shoulder dysfunction, and other seemingly unrelated symptoms—distant problems driven by central instability. When your core and pelvic floor don’t provide adequate stability, other areas of your body pick up the slack, eventually breaking down under demands they weren’t designed to handle.
Truth Three: Avoidance Strategies Guarantee Long-Term Problems
Being told “don’t lift, don’t run, don’t strain” might seem protective in the short term, but avoidance progressively reduces both your confidence and your tissue’s actual capacity to handle load.
The Avoidance Paradox:
SHORT-TERM: Avoidance reduces symptoms
↓
MEDIUM-TERM: Capacity decreases from lack of exposure
↓
LONG-TERM: Symptoms return when you eventually resume activity
When you eventually resume normal life, symptoms return because you haven’t built tolerance—you’ve only delayed the problem while simultaneously reducing your capacity. This creates a progressively narrowing window of tolerable activity.
Understanding Pelvic Floor Pain in Full Context
The Interconnected Nature of Pain Symptoms
Pelvic floor pain symptoms rarely exist in isolation. They commonly coexist with lower back pain, hip restriction or stiffness, abdominal wall dysfunction, and persistent protective posture patterns.
Treating pain locally without addressing these contributing factors severely limits your progress. Pain is an output of your entire nervous system’s assessment of threat, not just a local tissue problem.
Why Integrated Assessment Matters
When assessment looks only at the pelvic floor, it misses critical drivers of dysfunction. Your lower back might be creating compensatory demands. Your hip restriction might be altering how load moves through your pelvis. Your breathing pattern might be creating excessive downward pressure. Your protective postures might be maintaining muscle guarding patterns.
All of these factors contribute to pelvic floor pain, and all must be addressed for comprehensive resolution.
How Pelvic Floor Care Integrates With Broader Physiotherapy
The Connected System Approach
Pelvic floor physiotherapy doesn’t exist as an isolated treatment approach. It integrates with multiple aspects of musculoskeletal and nervous system care.
Connections to Other Treatment Areas:
Musculoskeletal Injury Treatment
When load distribution fails throughout your body, the pelvic floor often becomes part of the compensation pattern. Addressing injuries elsewhere in the kinetic chain frequently improves pelvic floor symptoms.
Pain Modulation Approaches
When pain modulation support is beneficial, techniques like electrotherapy can reduce nervous system sensitivity while you work on retraining movement patterns.
Movement Pattern Cueing
Dynamic and kinesiology taping can temporarily cue better movement patterns, helping your nervous system learn new coordination strategies.
Arthritis Management
Arthritis-related stiffness in the hips, spine, or pelvis alters pelvic mechanics in ways that can overload the pelvic floor. Managing joint health becomes part of managing pelvic floor function.
Tendinitis and Force Transfer
Tendinitis often develops when force transfer patterns are disrupted. These same disrupted patterns typically affect pelvic floor function, making treatment of both conditions interconnected.
These aren’t separate, unrelated problems—they’re interconnected aspects of how your whole body functions as an integrated system.
When to Seek Pelvic Floor Physiotherapy
Clear Indicators for Professional Assessment
Consider getting evaluated by a qualified pelvic floor physiotherapist when any of the following situations apply to you.
Persistent Symptoms Beyond Early Recovery
If symptoms persist beyond the early postpartum recovery period (typically 8-12 weeks), professional assessment can identify why normal healing hasn’t occurred and what’s perpetuating the dysfunction.
Exercises Haven’t Helped
When you’ve tried pelvic floor exercises consistently for 6-8 weeks without improvement, assessment can determine whether you’re doing the wrong exercises, doing them incorrectly, or whether exercises alone aren’t sufficient for your particular problem.
Daily Life Limitations
If pain, leakage, or pressure sensations are limiting your daily activities, work responsibilities, exercise participation, or sexual function, these symptoms warrant professional evaluation rather than continued self-management attempts.
Unpredictable Symptom Fluctuations
When symptoms fluctuate unpredictably without clear patterns related to your activities or cycle, assessment can help identify hidden triggers and contributing factors.
Fear-Driven Movement Choices
If fear has become the primary factor driving your movement choices—avoiding activities you want to do, constantly worried about symptoms, or progressively limiting your life—this indicates that professional guidance could help you build capacity and confidence.
What Quality Pelvic Floor Physiotherapy Actually Involves
Pelvic floor physiotherapy in Mississauga or anywhere else shouldn’t be about simply doing more exercises. The goal is restoring how your entire system behaves under the actual loads you face in daily life.
Quality care involves comprehensive assessment of the whole kinetic chain, identification of specific contributing factors to your symptoms, development of an individualized treatment plan, progressive exposure to build capacity, education about load management, and strategies for long-term self-management.
When Professional Care Becomes Necessary
If pelvic floor pain symptoms persist, intensify, or begin interfering with work, physical activity, or intimacy, a professional assessment is no longer optional—it’s essential. At this stage, care must move beyond symptom management and focus on identifying underlying contributors such as movement dysfunctions, breathing pattern faults, pressure mismanagement, and nervous system involvement.
Clinics like Get Back Physiotherapy address pelvic rehabilitation through evidence-based Pelvic Floor Physiotherapy in Mississauga, combining detailed pelvic assessment with whole-body movement analysis to support meaningful, long-term recovery rather than short-term relief.