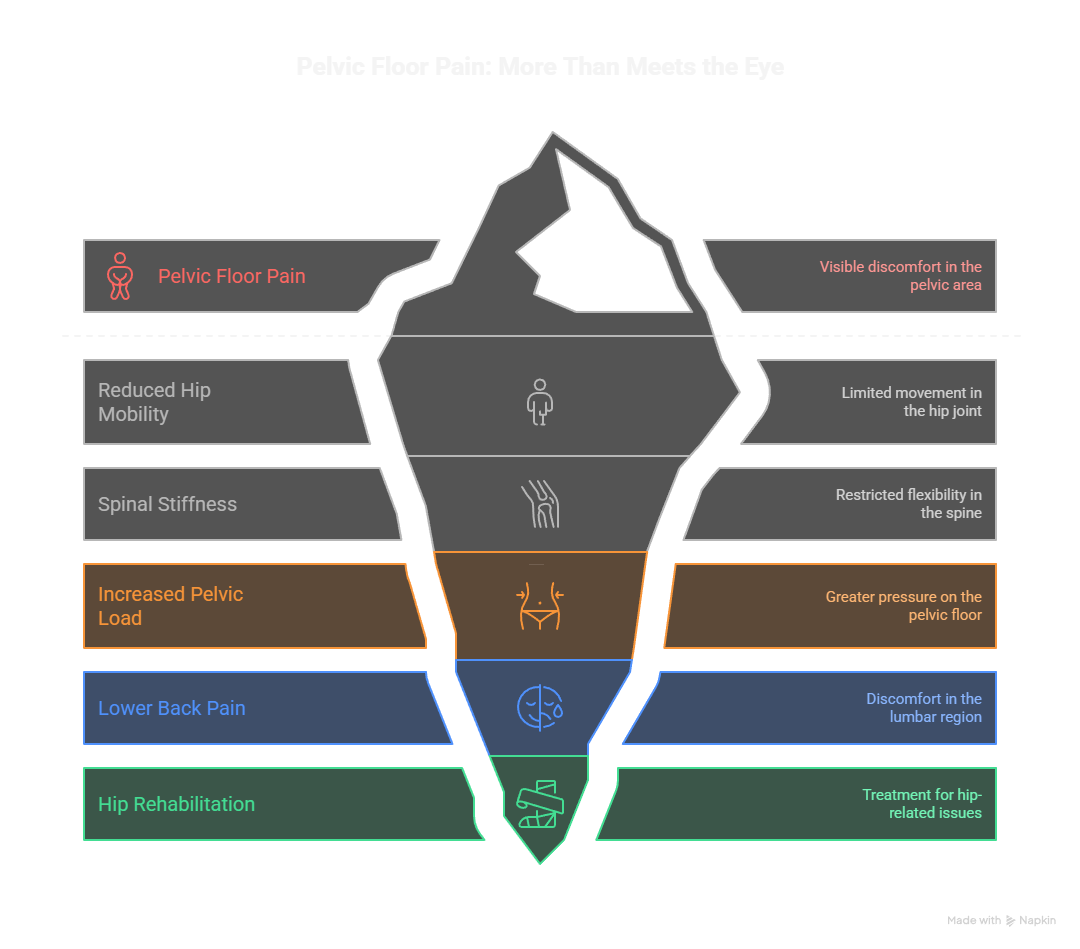
One of the biggest misconceptions about pelvic floor pain is that it exists in isolation. In clinical practice, pelvic symptoms almost always overlap with issues elsewhere in the body.
For example, reduced hip mobility or spinal stiffness can increase load on the pelvic floor during sitting, walking, or lifting. This is why many patients with pelvic pain also report symptoms commonly treated through
lower back pain physiotherapy
and hip-related rehabilitation.
Gap 1: Static symptom lists
Most resources treat symptoms as fixed problems. In reality, pelvic floor pain changes based on load, stress, hormones, sleep quality, and what the rest of your body is doing. Understanding these patterns is more valuable than memorizing symptom lists.
Gap 2: Linear recovery assumptions
Recovery is presented as a straight line from pain to no pain. Most people experience fluctuations, plateaus, and occasional setbacks. Without understanding this, temporary worsening causes unnecessary anxiety and treatment abandonment.
Gap 3: Isolated pelvic focus
The pelvic floor is treated as separate from the rest of the body. This ignores how interconnected your movement system actually is. Hip restrictions, breathing patterns, and spinal mobility all directly impact pelvic floor function.
What This Guide Covers
This comprehensive guide fills those gaps by explaining:
- Why pelvic floor pain behaves the way it does
- How symptoms change with different triggers and contexts
- When standard treatment approaches might make things worse
- How pelvic pain connects to issues in your hips, back, and even shoulders
- What recovery actually looks like in practice
- How to assess whether you need immediate professional help
- Specific strategies for different life situations
Who This Guide Is For
You’ll benefit from this guide if you are:
- Experiencing persistent pelvic discomfort or pain
- Someone who’s tried pelvic floor exercises without improvement
- Dealing with pain after childbirth, surgery, or injury
- Noticing your pelvic pain seems connected to other body issues
- Wanting to understand your symptoms before seeking treatment
- A partner or family member trying to understand what your loved one is experiencing
- Preparing for pregnancy and want to prevent problems
- An athlete experiencing pelvic symptoms with training
Pain When Sitting: A Key Diagnostic Pattern
Pain that builds after 15–30 minutes of sitting is one of the most common pelvic floor complaints. People often describe deep aching, burning, or the sensation of “sitting on a golf ball.”
Clinically, this pattern suggests:
- Compression intolerance
- Nervous system sensitivity
- Poor load distribution through the hips and spine
Because of this overlap, sitting intolerance is frequently addressed alongside
hip pain physiotherapy
and postural re-education rather than isolated pelvic strengthening.
The pelvic floor has five primary functions:
Organ Support: These muscles support your bladder, bowel, and reproductive organs, keeping them in proper position against gravity and intra-abdominal pressure.
Sphincter Control: They control when you urinate and have bowel movements, allowing you to hold or release at appropriate times.
Sexual Function: The pelvic floor contributes to sexual arousal, sensation, and orgasm in both men and women.
Core Stability: Working with your diaphragm, deep abdominal muscles, and back muscles, the pelvic floor is integral to spinal stability and posture.
Pressure Management: These muscles respond to changes in intra-abdominal pressure from activities like coughing, sneezing, laughing, and lifting.
Why Pelvic Floor Pain Is So Complex
Unlike pain in an isolated joint like a knee or elbow, pelvic floor pain involves multiple interconnected systems:
Multiple tissue types: Muscles, nerves, fascia, blood vessels, and organs all exist in close proximity. Pain in one tissue can affect others.
Hormonal influences: Especially in women, hormonal fluctuations during menstrual cycles, pregnancy, and menopause significantly affect tissue response, pain sensitivity, and healing capacity.
Nervous system sensitivity: After prolonged pain (typically 3-6 months), the nervous system can become oversensitive, amplifying pain signals even when tissue healing has occurred.
Whole-body mechanics: How you move, breathe, and distribute load throughout your body directly affects the pelvis. Restrictions in your hips, spine, or ribcage force the pelvic floor to compensate.
Psychological factors: Stress, trauma history, and anxiety directly affect pelvic floor tension. The mind-body connection is particularly strong in the pelvic region.
The Variable Nature of Pelvic Pain
Pelvic floor pain is rarely constant. Understanding when and why your pain changes provides crucial diagnostic information.
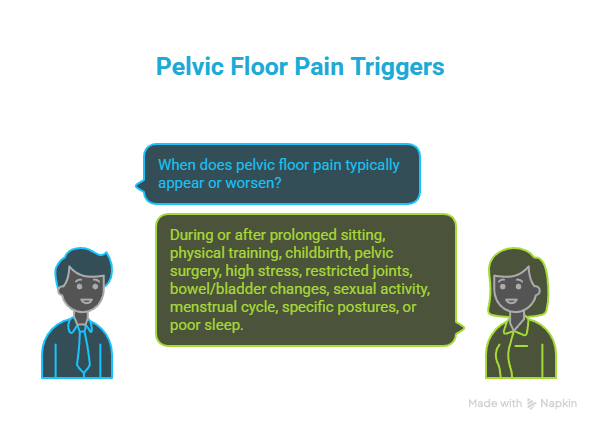
Pain typically appears or worsens:
- During or after prolonged sitting (especially beyond 30 minutes)
- Following physical training, exercise, or increased activity
- After childbirth or during pregnancy
- Following pelvic or abdominal surgery
- During high-stress periods or anxiety episodes
- When other joints (hips, lower back) become restricted or painful
- With changes in bowel or bladder function (constipation, urgency)
- During or after sexual activity
- At specific times during the menstrual cycle
- With certain postures or movements (bending, lifting, twisting)
- After poor sleep or during periods of fatigue
This variability is a diagnostic clue, not a sign that symptoms are “in your head.” The pattern of when pain occurs tells us what’s driving it and guides treatment decisions.
Quick Symptom Recognition
| Symptom Type | What It Feels Like | Common Triggers | What It Usually Indicates | Urgency Level |
| Sitting Pain | Deep aching or burning after 15-30 min; “sitting on a golf ball” | Desk work, driving, long meetings | Nervous system sensitivity, compression intolerance | Monitor |
| Pelvic Pressure | Heaviness, dragging sensation; “everything falling out” | End of day, after standing, lifting | Muscle coordination issues, possible prolapse | Assess |
| Post-Childbirth Pain | Scar sensitivity, deep aching, pain with intimacy | Lifting baby, bending, intercourse | Tissue healing, compensation patterns | Monitor |
| Pregnancy Pain | Pubic or tailbone pain, pain with walking/stairs | Weight bearing, position changes | Adaptation challenges, joint instability | Assess |
| Post-Surgical Pain | Sharp or burning near scars, deep pelvic ache | Movement, scar stretching | Nerve healing, scar restrictions | Monitor |
| Bowel/Bladder Pain | Pain during or after elimination, incomplete emptying | Urination, bowel movements | Muscle hypertonicity, nerve sensitivity | Assess |
| Intimacy Pain | Pain with penetration or deep pelvic pain after | Sexual activity | Muscle tension, scar tissue, nerve sensitivity | Monitor |
| Unexplained Pelvic Ache | Constant or intermittent deep pelvic discomfort | Variable or unclear | Multiple possible causes | Assess |
| Sharp Stabbing Pain | Sudden sharp pain in pelvis or genitals | Random or with specific movements | Nerve irritation, muscle spasm | Assess |
| Radiating Pain | Pain spreading to thighs, buttocks, or abdomen | Various activities | Nerve involvement, referred pain | Urgent if progressive |
Urgency Key:
- Monitor: Track patterns, use self-care, seek help if worsening or lasting >6 weeks
- Assess: Schedule professional evaluation within 2-4 weeks
- Urgent: Seek medical attention within days
Detailed Symptom Analysis
1. Pain When Sitting (Sitting Intolerance)
What you might experience:
Deep aching or burning in the pelvis that begins after 15-30 minutes of sitting. Many people describe the sensation of “sitting on a golf ball,” “sitting on broken glass,” or “sitting on a hot coal.” The pain typically improves quickly when standing or walking, but returns and worsens as the day progresses. Some people find certain surfaces worse than others.
Commonly blamed on: Poor posture, weak pelvic floor muscles, or “just the way you’re sitting”
What’s actually happening:
- Reduced tolerance to sustained compressive load: The tissues cannot handle prolonged pressure without pain signals
- Limited hip mobility affecting pelvic mechanics: Stiff hips force the pelvis to absorb more load during sitting
- Heightened nervous system sensitivity: The nerves in the pelvic region have become oversensitive to pressure
- Reduced blood flow during static positions: Sustained compression limits circulation, causing tissue irritation
- Nerve irritation from sustained pressure: Direct compression on pudendal or other pelvic nerves
Why this pattern matters: Sitting pain that improves with movement but worsens with sustained positions is rarely about muscle weakness. It typically indicates nervous system involvement and often overlaps with hip pain physiotherapy and lower back pain physiotherapy, even when these connections aren’t initially obvious.
What helps: Position changes every 20-30 minutes, cushions that reduce direct pressure, addressing hip mobility, nervous system desensitization techniques.
2. Pelvic Pressure Without Clear Medical Findings
What you might experience:
A sensation of heaviness or dragging in the pelvis, often described as “everything is falling out” or “something is dropping down.” The pressure typically worsens by the end of the day, after prolonged standing, or with lifting activities. It usually improves significantly when lying down. You might feel the need to support the area with your hand.
What tests often show: Normal imaging (ultrasound or MRI), or mild findings that don’t correlate with symptom severity
What’s actually happening when imaging is normal:
- Delayed muscle relaxation: Muscles aren’t “switching off” properly after contracting, maintaining constant tension
- Poor breathing-pelvic coordination: The diaphragm and pelvic floor aren’t working together rhythmically
- Sensory amplification: The nervous system is over-interpreting normal sensations as problematic
- Increased muscle tone rather than structural prolapse: Muscles are too tight, creating a sensation of pressure
Why this distinction matters: Early labels like “prolapse” can lead to unnecessary surgical interventions when the actual issue is functional coordination, not structural damage. Many people with minimal imaging findings have severe symptoms, while others with significant imaging findings have no symptoms at all.
What helps: Breathing retraining, pelvic floor relaxation techniques, posture variability, addressing muscle tone rather than strengthening.
Pelvic Pain After Childbirth
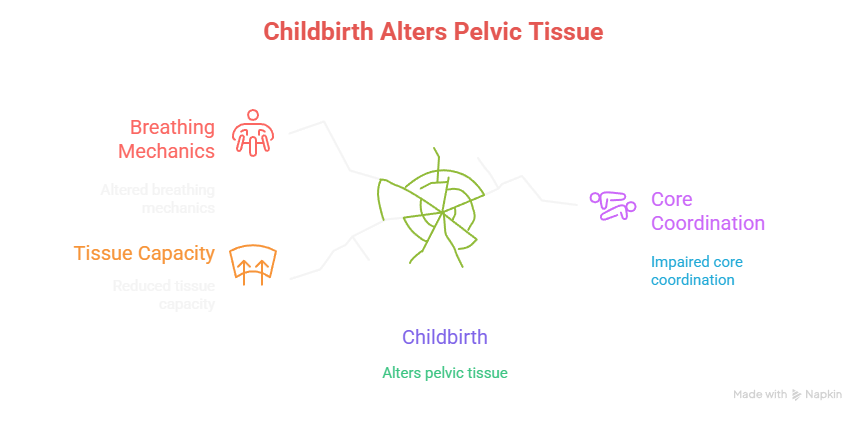
Postpartum pelvic pain is often dismissed as something that will “resolve with time.” In reality, childbirth alters tissue capacity, breathing mechanics, and core coordination far beyond the initial recovery window.
Successful postpartum recovery follows the same graded principles used in
pre and post operative rehab,
focusing on restoring movement confidence, breathing efficiency, and load tolerance instead of rushing into aggressive strengthening.
What actually changes after childbirth:
Tissue load tolerance: Your tissues need time to heal and rebuild capacity to handle normal loads. This process takes longer than the traditional “6-week clearance” suggests.
Sleep quality and recovery capacity: Poor sleep directly impairs tissue healing and increases pain sensitivity. The chronic sleep deprivation of new parenthood significantly impacts recovery.
Core muscle coordination: Your abdominal and pelvic floor muscles need to relearn how to work together after pregnancy stretched and separated them.
Pelvic floor compensation patterns: Some muscles become overactive trying to compensate for others that aren’t working well, creating imbalances.
Altered breathing mechanics: Holding and feeding a baby changes your breathing patterns, which affects pelvic floor function.
Critical insight: Successful postpartum recovery requires whole-body rehabilitation, not just pelvic floor exercises. This follows the same principles used in pre and post operative rehab. The traditional “just do Kegels” advice often fails because it addresses only one piece of a complex puzzle.
What helps: Graded return to activities, addressing sleep when possible, whole-body movement retraining, scar tissue mobilization, breathing pattern restoration.
4. Pain During Pregnancy (Prenatal Pelvic Pain)
What you might experience:
- Pubic symphysis pain (sharp pain at the front of your pelvis)
- Sacroiliac joint pain (deep ache at the back of your pelvis, one or both sides)
- Deep pelvic aching that worsens with walking
- Difficulty rolling in bed or getting out of a car
- Pain with stairs, one-legged activities, or prolonged standing
Why it’s often dismissed: “Pain is normal during pregnancy” or “it will go away after delivery”
What pregnancy actually changes:
Ligament behavior and joint stability: The hormone relaxin loosens ligaments to prepare for birth, but this also reduces stability throughout the pelvis and spine.
Breathing mechanics: As the baby grows, your diaphragm can’t descend as far, which changes how your entire core system works.
Center of mass and weight distribution: Your weight shifts forward, changing how forces travel through your body and increasing demand on your lower back and pelvic floor.
Pain sensitivity: Pregnancy can increase or decrease pain sensitivity depending on individual factors and stage of pregnancy.
Load distribution through the pelvis: The growing baby changes how weight is distributed across your pelvic joints.
Critical insight: Pelvic pain during pregnancy usually signals that your body is struggling to adapt to these changes, not that pain is inevitable. The earlier you address it, the easier it is to manage. Waiting until after delivery often makes recovery significantly harder and longer.
What helps: Pelvic support garments when appropriate, activity modification, specific strengthening of muscles that support the pelvis, manual therapy for restricted joints, education on optimal positions.
5. Pain After Surgery (Post-Surgical Pelvic Pain)
Common after these procedures:
- Hysterectomy (removal of uterus)
- Cesarean section
- Hernia repair (inguinal or abdominal)
- Prostate surgery (prostatectomy)
- Endometriosis excision
- Pelvic organ prolapse repair
- Bladder or bowel surgery
What drives post-surgical pain:
Scar tissue stiffness: Scars restrict movement of underlying tissues. Even internal scars you can’t see can create restrictions that cause pain.
Altered nerve signaling: Nerves that were cut or stretched during surgery heal slowly and may send abnormal signals during the healing process.
Protective muscle guarding: Your body automatically tenses muscles around a surgical site to protect it, but this guarding can persist long after healing.
Reduced load tolerance: Surgically altered tissues can’t initially handle the same loads as before surgery.
Changes in tissue mobility: Surgery changes how tissues glide and move against each other.
Why standard approaches fail: Treating only the pelvic floor misses the underlying drivers. Post-surgical pain overlaps heavily with chronic pain mechanisms seen throughout the body. The surgery has changed the mechanical and neurological environment, requiring a comprehensive approach.
What helps: Scar tissue mobilization (both external and internal), graded exposure to movement, nervous system education, addressing compensatory patterns in surrounding areas.
6. Pain With Bowel or Bladder Function
What you might experience:
- Sharp or burning pain with urination
- Discomfort immediately after emptying your bladder
- Pain with bowel movements, especially with straining
- Sensation of incomplete emptying despite just going
- Urgency to urinate or defecate without infection
- Hesitancy or difficulty initiating elimination
- Pain that radiates to the rectum or urethra
What this often indicates:
Pelvic floor muscle hypertonicity: The muscles are too tight and can’t relax properly to allow comfortable elimination.
Nervous system sensitization: The nerves around the bladder or bowel have become oversensitive, interpreting normal sensations as pain.
Poor coordination of pelvic floor relaxation: The muscles should relax during elimination, but instead they contract or stay tense.
Fascial restrictions: The connective tissue around organs has become restricted, limiting normal organ movement.
Red flags requiring immediate medical assessment:
- Blood in urine or stool
- Fever accompanying urinary symptoms
- New onset incontinence (leaking when you weren’t before)
- Complete inability to empty bladder or bowel
- Severe pain with elimination
- Unexplained weight loss with bowel symptoms
What helps: Pelvic floor relaxation techniques, bowel and bladder habit retraining, addressing constipation, internal manual therapy, biofeedback to learn proper muscle coordination.
7. Pain With Intimacy (Dyspareunia)
What you might feel:
- Sharp pain with initial penetration
- Deep pelvic pain during intercourse
- Burning or stinging sensations
- Muscle spasms during or after activity
- Aching that persists for hours or days after
- Anxiety or fear about intimacy due to pain
Common contributing factors:
Muscle hypertonicity: Pelvic floor muscles are too tight and resist penetration, causing pain.
Scar tissue from childbirth or surgery: Scars at the vaginal opening or deeper tissues create restrictions and sensitivity.
Nervous system sensitization: Previous painful experiences have taught the nervous system to expect pain, amplifying signals.
Hormonal changes affecting tissue health: Low estrogen (postpartum, breastfeeding, menopause) causes tissue thinning and reduced lubrication.
Psychological factors: Past trauma, current anxiety, or relationship stress can increase muscle tension.
Inadequate arousal or lubrication: Rushing or insufficient foreplay leads to increased friction and discomfort.
Why this matters: Sexual pain is treatable and deserves the same clinical attention as any other pain condition. It’s not “just psychological” and it’s not something you have to accept or live with. The psychological component is real and valid, but it’s part of a complex picture that includes tissue health, muscle function, and nervous system behavior.
What helps: Dilator therapy for gradual desensitization, pelvic floor muscle relaxation, hormone therapy when appropriate, counseling for psychological factors, communication strategies with partners, pain education to reduce fear.
Gender-Specific Considerations
Pelvic Floor Pain in Women
Unique contributing factors:
Hormonal fluctuations: Estrogen, progesterone, and other hormones affect tissue response, pain sensitivity, and healing capacity throughout the menstrual cycle, during pregnancy, and through menopause.
Pregnancy and childbirth: These fundamentally alter tissue integrity, load distribution, and muscle coordination. Even uncomplicated pregnancies and deliveries create significant physical demands.
Historical dismissal of symptoms: Women’s pain has historically been minimized, attributed to psychological causes, or labeled as “normal” when it’s actually treatable.
Higher incidence of specific conditions: Endometriosis, interstitial cystitis, and vulvodynia occur almost exclusively in women and often coexist with pelvic floor dysfunction.
More complex anatomy: The proximity of reproductive, urinary, and digestive organs in a smaller space creates more potential for symptom overlap and complexity.
Most common presentations in women:
- Postpartum pain (affects 40-60% to some degree)
- Menstrual cycle-related pain patterns
- Menopausal changes affecting tissue health
- Pain after gynecological procedures
- Chronic pelvic pain of unclear origin
Pelvic Floor Pain in Men
Unique contributing factors:
Later symptom onset: Men typically experience pelvic floor issues later in life, often in their 40s-60s.
Common activity-related triggers: Prolonged sitting (office work, driving), cycling, and certain sports create specific patterns of pain.
Significant diagnostic delay: On average, men wait 2-3 years before receiving proper pelvic floor assessment because awareness is lower and symptoms are often attributed to prostate issues first.
Prostate involvement often suspected first: Many men undergo extensive prostate testing before pelvic floor dysfunction is considered, leading to delayed treatment.
Less cultural acceptance: Men may feel stigmatized discussing pelvic pain, urinary symptoms, or sexual dysfunction, delaying help-seeking.
Most common presentations in men:
- Chronic prostatitis/chronic pelvic pain syndrome (CPPS)
- Post-prostatectomy pain or incontinence
- Cyclist-related pelvic pain (pudendal neuralgia)
- Occupational sitting-related pain (truck drivers, office workers)
- Post-hernia repair pain
Key insight for both genders: The meaningful difference between men and women is exposure patterns, timing, and systemic context rather than anatomy alone. The underlying principles of assessment and treatment remain largely the same: address muscle function, nervous system sensitivity, mechanical contributors, and whole-body patterns.
Advanced Clinical Concepts
Why Strengthening Can Make Pain Worse
This is an uncomfortable truth that many practitioners don’t explain clearly, but it’s crucial for understanding why “just do Kegels” often fails or worsens symptoms.
When pain is primarily driven by:
- Muscle overactivity (muscles that can’t relax)
- Poor muscle relaxation patterns
- Nervous system threat sensitivity
- Excessive baseline muscle tone
Strengthening exercises can:
- Increase compression and pressure on already irritated tissues
- Elevate muscle tone even further above baseline
- Intensify symptom presentation
- Create more protective guarding patterns
- Reinforce dysfunctional movement strategies
The fundamental principle: You cannot effectively strengthen a muscle that won’t relax properly first. A muscle that stays partially contracted can’t generate full force, and attempting to strengthen it only increases the dysfunction.
This mirrors what happens in tendinitis and chronic pain rehabilitation when loading is applied without proper capacity assessment. The tissue isn’t ready for the demand, and the intervention worsens the problem.
What to do instead: Begin treatment with relaxation techniques, breathing coordination, nervous system regulation, and restoring normal muscle resting tone before progressing to strengthening. For many people with pelvic floor pain, the entire treatment focuses on learning to relax and coordinate muscles rather than making them stronger.
How to know which you need:
- If you can’t fully relax your pelvic floor, you need relaxation work first
- If you leak with all exertion regardless of effort, you might need strengthening
- If symptoms worsen with any exercise attempt, stop strengthening and focus on coordination
The Pelvic Floor Never Fails Alone
Pelvic pain frequently coexists with other musculoskeletal complaints. It is not uncommon for patients to also experience:
- knee pain physiotherapy needs due to altered load transfer
- shoulder pain physiotherapy from compensatory tension patterns
- Overuse injuries addressed through
musculoskeletal injuries treatment
This full-body compensation explains why isolated pelvic exercises often fail to resolve symptoms completely.
The interconnected movement system:
Stiff hips: When hip mobility is limited, the pelvis must move more during activities like walking, squatting, and bending. This excessive motion overworks the pelvic floor and creates compensation patterns.
Limited spinal mobility: A stiff mid-back (thoracic spine) or lower back forces the pelvis to absorb more load during daily activities. The pelvic floor works harder to stabilize.
Altered breathing patterns: The diaphragm and pelvic floor move together rhythmically. Chest breathing, breath holding, or poor breathing patterns directly affect pelvic floor function and create abnormal pressure patterns.
Restricted thoracic expansion: Limited rib cage movement affects breathing mechanics and changes how pressure is managed through the core system.
Foot and ankle restrictions: How force travels up from the ground is altered by foot and ankle problems. The pelvis must compensate for poor shock absorption lower in the chain.
Jaw tension: Surprisingly, jaw tension and pelvic floor tension are neurologically linked. People who clench their jaw often unconsciously tense their pelvic floor simultaneously.
Clinical observation: Pelvic pain often coexists with knee pain, hip pain, shoulder pain, or even jaw pain that seem completely unrelated. This isn’t coincidence—it’s the body compensating across multiple regions.
Why this matters profoundly: Treating only the pelvic floor while ignoring these contributing factors explains why many people see initial improvement that plateaus after 2-3 months or regresses when they return to normal activities. The system hasn’t been fully addressed.
Treatment implications: Effective pelvic floor rehabilitation must assess and address hip mobility, spinal function, breathing patterns, and foot mechanics alongside direct pelvic floor work. This is the approach used in clinics like Get Back Physiotherapy, where pelvic symptoms are assessed as part of comprehensive movement analysis rather than isolated muscle problems.
The Nervous System’s Role in Persistent Pain
After approximately 3-6 months of pain, neurological changes occur that can maintain pain even after tissues have healed. Understanding this prevents frustration and guides appropriate treatment.
How pain becomes chronic:
Peripheral sensitization: Nerve endings in the tissues become more sensitive, sending stronger pain signals for the same stimulus.
Central sensitization: The spinal cord and brain become more sensitive to all incoming signals, amplifying pain messages.
Cortical reorganization: The brain’s body map changes, sometimes expanding the representation of painful areas.
Reduced pain inhibition: The body’s natural pain suppression systems become less effective.
Signs your nervous system is involved:
- Pain that seems out of proportion to any identifiable tissue damage
- Pain that spreads to new areas beyond the original problem
- Increased sensitivity to touch, pressure, temperature, or even clothing
- Pain that varies dramatically with stress levels or sleep quality
- Multiple areas of body pain, not just the pelvis
- Pain that responds strongly to context (better on vacation, worse at work)
- Allodynia (pain from normally non-painful stimuli like light touch)
What this means for treatment: Later-stage pelvic pain requires nervous system-focused approaches including:
- Graded exposure to previously painful activities
- Stress management and relaxation training
- Sleep optimization strategies
- Pain neuroscience education to understand pain mechanisms
- Reducing fear and catastrophic thinking about pain
- Mindfulness or other mind-body techniques
The good news: Understanding that your pain involves nervous system changes is empowering, not dismissive. It means your pain is real, explainable, and treatable through specific approaches that target these mechanisms.
Long-Term Consequences of Ignoring Pelvic Floor Pain
Most resources stop at describing symptoms and suggesting treatment. Here’s what can develop when pain is left unaddressed for extended periods:
Physical consequences:
Nervous system sensitization: Pain becomes easier to trigger with less and less stimulus. Activities that once caused mild discomfort now cause significant pain.
Muscle atrophy and deconditioning: Avoidance of activities leads to loss of muscle mass and cardiovascular fitness, creating a downward spiral of reduced capacity.
Compensatory movement patterns: The body develops inefficient ways of moving to protect the painful area. These patterns become habitual and create problems in other joints.
Chronic postural adaptations: Sustained protective postures (hunching, tilting, guarding) become structural over time, requiring more intensive intervention to reverse.
Functional consequences:
Activity avoidance and reduced participation: Gradually withdrawing from activities you love, social events, exercise, and hobbies that trigger symptoms.
Fear-based movement patterns: Moving as if you’re fragile, which paradoxically increases injury risk and reinforces the pain experience.
Decreased tolerance to normal daily activities: Progressively losing the ability to perform basic tasks like prolonged sitting, walking, or lifting without symptom provocation.
Impact on work capacity and career: Difficulty fulfilling job requirements, taking frequent sick days, or making career changes due to symptoms.
Psychological consequences:
Anxiety around symptom triggers: Constantly monitoring for and worrying about what might cause pain, which increases overall stress.
Depression from chronic limitations: Loss of hope, feelings of helplessness, and mood disturbances from ongoing restrictions.
Relationship strain: Impact on intimacy, reduced social engagement, and stress on partners who don’t fully understand the condition.
Loss of identity and confidence: Feeling defined by pain rather than by your interests, roles, and accomplishments.
At this stage: Rehabilitation shifts from true recovery to symptom management and learning to live with limitations. While improvement is still possible, it requires significantly more time, effort, and interdisciplinary care. Early intervention prevents this progression entirely.
When to Seek Professional Help
Understanding when to seek help prevents both unnecessary delays and premature panic. Here’s a clear framework:
Seek Immediate Medical Attention (Emergency Room or Call Emergency Services)
Medical emergencies requiring same-day evaluation:
- Sudden complete inability to urinate or defecate
- Loss of sensation in the genital area, inner thighs, or buttocks (saddle anesthesia)
- New onset loss of bladder or bowel control (incontinence that came on suddenly)
- Severe pelvic pain accompanied by fever above 101°F (38.3°C)
- Heavy unexplained vaginal or rectal bleeding
- Severe pain following recent trauma or injury to the pelvis
- Signs of infection after recent surgery (fever, severe pain, foul-smelling discharge)
Why these are emergencies: These symptoms can indicate cauda equina syndrome (spinal cord compression), severe infection, or other conditions requiring immediate medical intervention to prevent permanent damage.
Seek Professional Assessment Within 48-72 Hours
Urgent concerns requiring prompt evaluation:
- Pain that consistently wakes you from sleep multiple nights
- Progressive worsening of symptoms over 2-4 weeks despite rest
- Pain accompanied by unexplained weight loss (more than 5-10 pounds unintentionally)
- New neurological symptoms (numbness, tingling, weakness in legs)
- Pain after recent surgery with concerning changes (increasing rather than decreasing pain, new symptoms)
- Inability to perform essential daily activities or work due to pain
- Pain with concerning additional symptoms (night sweats, persistent fever, extreme fatigue)
Why urgency matters: These patterns can indicate conditions that need medical workup to rule out infection, nerve compression, or other issues that respond better to early treatment.
Schedule Professional Evaluation Within 2-4 Weeks
Non-urgent but important situations:
- Pain lasting more than 6-8 weeks despite self-care attempts
- Pain that limits your ability to work, exercise, or engage in desired activities
- Symptoms that aren’t improving or are slowly worsening
- Pain that significantly affects your relationships or intimacy
- Confusion about what’s causing your symptoms or what to do
- Previous treatment that didn’t provide adequate improvement
- Desire to return to activities but unsure how to progress safely
- Pain during pregnancy (don’t wait until postpartum)
- Preventive assessment if you’re planning pregnancy and have risk factors
Why assessment helps: Early professional guidance prevents the development of chronic pain patterns, addresses problems while they’re simpler to treat, and provides clear direction rather than months of trial and error.
What “Waiting and Seeing” Risks
Many people delay seeking help, hoping symptoms will resolve on their own. While some acute issues do improve with rest, here’s what delayed care risks:
- Nervous system sensitization making pain harder to treat later
- Development of compensatory movement patterns throughout the body
- Progression from acute to chronic pain (changes after 3-6 months)
- Increased complexity of treatment needed
- Longer overall treatment duration
- Greater impact on work, relationships, and quality of life
- Higher healthcare costs in the long run due to more intensive treatment needs
The optimal window: Addressing pelvic floor pain within the first 3 months offers the best outcomes with the least intervention required.
Treatment Approaches That Actually Work
Effective pelvic floor pain treatment is rarely a single intervention. It requires comprehensive assessment and multi-faceted approach.
The Comprehensive Assessment Process
A thorough evaluation forms the foundation of successful treatment. Good assessment examines:
Pain pattern analysis:
- When does pain occur (time of day, specific activities)?
- What makes it better or worse?
- How has it changed since it started?
- What’s your pain like hour by hour, day by day?
Movement quality throughout the body:
- Hip mobility and strength
- Spinal segmental movement
- Breathing patterns
- Foot and ankle function
- Shoulder and thoracic mobility
Pelvic floor specific assessment:
- Can the muscles contract effectively?
- More importantly, can they relax fully?
- Is coordination with breathing present?
- Are there tender points or trigger points?
- What’s the resting muscle tone?
Contributing factors:
- Sleep quality and quantity
- Stress levels and management
- Bowel and bladder habits
- Exercise and activity levels
- Occupational demands (sitting, lifting, etc.)
- Previous injuries or surgeries
- Trauma history if relevant
Nervous system sensitivity:
- How does pain respond to stress?
- Are symptoms spreading?
- Is there heightened sensitivity to touch?
- What’s the pain experience like (burning, aching, sharp)?
Evidence-Based Treatment Components
- Pelvic Floor Muscle Training (Appropriate to Your Needs)
Not everyone needs strengthening. Training includes:
- Learning to identify and isolate pelvic floor muscles
- Relaxation techniques and “letting go” of unnecessary tension
- Coordination with breathing (exhale with relaxation, inhale with gentle lift)
- Strengthening only when appropriate and after relaxation is established
- Functional integration into daily
When Professional Care Matters
If pelvic pain persists, worsens, or begins affecting work, exercise, or intimacy, professional assessment is essential. Structured evaluation looks beyond symptoms to identify movement faults, breathing dysfunction, and nervous system involvement.
Clinics like Get Back Physiotherapy approach pelvic rehabilitation through evidence-based Pelvic Floor Physiotherapy Mississauga, integrating pelvic assessment with whole-body movement analysis for sustainable recovery.